The Duties and Responsibilities of the Radiation Safety Officer

In this week’s video, Eric from Olympic Health Physics provides an overview of the duties and responsibilities of the RSO or Radiation Safety Officer.
This video covers the regulatory requirements and expectations of a medical RSO following the guidance in NUREG 1556, Vol. 9, Rev. 3. that is specific to medical licensees.
What Is a Radiation Safety Officer?
The Radiation Safety Officer or RSO is the person within a medical licensee facility who is responsible for overseeing and implementing the radiation safety program. They are the ones responsible for ensuring that the facility is compliant with all of the regulations and overseeing that radiation safety program.
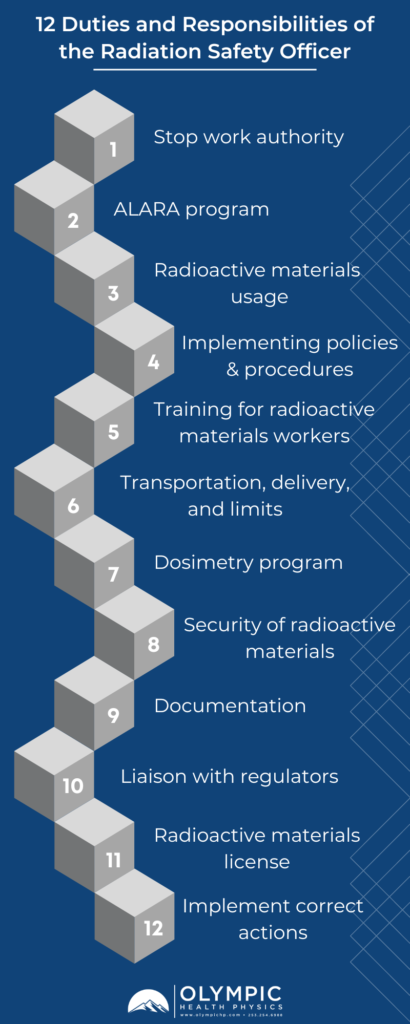
Twelve General Duties and Responsibilities of the RSO
We’re going to go through some of the typical duties and responsibilities of the Radiation Safety Officer. It’s important to note there can be many additional duties assigned to the RSO. Below, we outline twelve general duties of the Radiation Safety Officer in relation to the regulatory requirements and expectations of a medical RSO following the guidance in NUREG 1556, Vol. 9, Rev. 3. that is specific to medical licensees.
1. Stop Work Authority
The first duty of the Radiation Safety Officer is Stop Work Authority. What does this mean?
It means that the Radiation Safety Officer has the ability to stop any work involving radioactive materials. This is usually spelled out in what’s called a Delegation of Authority that comes from the facilities administration and assigned by facility administration, as well as the Radiation Safety Officer. Stop Work Authority is usually used whenever there are unsafe work practices and something needs to be fixed or changed before the work can continue.
2. Overseeing the ALARA Program
The Radiation Safety Officer has a responsibility to ensure that radioactive doses are kept ALARA. ALARA is an acronym that stands for As Low As Reasonably Achievable. Within the facility, the RSO is responsible for ALARA and implementing an ALARA program.
3. Managing Radioactive Materials Usage
They also oversee all radioactive materials uses, including monitoring and surveying of all areas where radioactive materials are either used or stored.
4. Implementing Policies and Procedures
The RSO is responsible for drafting and implementing policies and procedures that deal specifically with the security of radioactive material, emergency procedures and operations that employ radioactive materials.
5. Training For Workers Handling Radioactive Materials
The Radiation Safety Officer typically conducts training for radioactive materials workers. They’re going to be providing training about the use and safety of radioactive materials within the facility.
6. Transportation, Delivery, and Radioactive Materials Limits
They are also responsible for the safe transportation and delivery of radioactive materials. The RSO ensures the packages are checked in properly, that there are surveys of packages and all deliveries are documented. Radiation Safety Officers also ensure that the facility’s possession limits are adhered to. The possession limits are outlined in the radioactive materials license for the facility. The RSO is responsible for making sure that the facility doesn’t exceed radioactive material possession limits.
7. Dosimetry Program
The RSO is also going to oversee and potentially implement the dosimetry program. Dosimetry is how we measure or monitor radiation doses, such as occupational radiation exposure, for staff.
8. Security of Radioactive Materials
Security of radioactive materials fall under the jurisdiction of the Radiation Safety Officer to ensure that any radioactive material is going to be secured from unauthorized removal. This is typically done in one of two ways. Either the radioactive material is going to be under lock and key of some sort, or it can also be under constant surveillance. So the radiation safety officer will be responsible for making sure that radioactive materials are secured in one of these two ways.
9. Documentation of the Radiation Safety Program
Documentation is a really big topic because any time we’re dealing with radioactive materials, we have to document most of the processes that go with them. Some of the documentation include surveys, inventory, receipt, and disposal of waste. All of these activities should be documented.
10. Liaison With Regulators
They’re also going to serve as a liaison with regulators and report any medical events or anything that’s a reportable event. The RSO will report events either to the state, if they’re in agreement state or to the NRC, if they’re not in an agreement state.
11. Managing the Radioactive Materials License
The Radiation Safety Officer may manage the radioactive materials license. This can include implementing any license conditions within the radioactive materials license, as well as submitting any amendments to the regulatory agency for changes to the license. Amendments are typically going to be for things like:
• changing an authorized user
• changing the radiation safety officer
• changing the address of the facility
• changing the name of the facility
• changing the proposed uses or the locations of those uses
All the above are typical things that would require submitted amendments.
12. Implement Corrective Actions
And lastly, the RSO implements any corrective actions for deficiencies or inefficiencies that are found in a radiation protection program, audits or external inspection conducted by a regulatory agency.
So this gives you a high level overview of the duties and responsibilities of the Radiation Safety Officer. The RSO may have more duties than what we’ve listed here. It’s usually up to the organization on what those responsibilities and duties will be for the RSO, but this will give you a pretty good place to start to understand the role of an RSO.
Questions and comments about RSO duties? Feel free to shoot them over to us. We’ll be happy to respond to any questions or comments that you have around Radiation Safety Officers and be a resource for you.
Our team is dedicated to ensuring that your facilities’ radiation safety program functions in accordance to regulatory standards, sound radiation safety principles, and most importantly serves to protect staff, patients, and the general public from the hazards associated with ionizing radiation. To this end, Olympic Health Physics can provide a physicist to your organization to fulfill the Duties of the Radiation Safety Officer. To learn more, check out our RSO Services or click the link below.